Computer modeling is helping researchers battle COVID-19.
Paul Macklin, an associate professor at the Luddy School of Informatics, Computing, and Engineering, is leading an international COVID-19 simulation group to rapidly build a SARS-CoV-2 tissue simulator with a group of virologists, pharmacologists, and mathematicians.
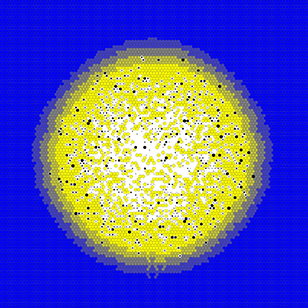
Macklin’s previous research has focused on developing PhysiCell, a 3D computer modeling system that has previously been used to study cancer biology, nanotherapy, tissue engineering, immunology, and more. The SARS-Cov-2 tissue simulator is a rapid prototyping project that aims to create multiscale simulation models to shed light on the emergent dynamics that lead to divergent outcomes, identify actionable “choke points” for pharmacologic interactions, screen potential therapies, and identify potential biomarkers that differentiate response dynamics.
“I saw a several mathematicians and pharmacologists on Twitter talking about possibly modeling SARS-CoV-2 dynamics in tissue, and Thomas Hillen at the University of Alberta assembled a COVID-19 physiology reading group,” Macklin said. “Our lab had already been developing similar models of nanoparticles moving through tissues and entering cells through the nanoBIO project, oncolytic virus therapies with Morgan Craig and Adrianne Jenner at the University of Montreal, and demonstration models of viral replication and macrophages. I realized that there was an acute need to model dynamics, and that it would be very feasible to build on all this prior expertise to simulate SARS-CoV-2 in human tissues. I also thought we could build a proof of concept prototype very quickly.”
Along with colleagues from the University of Montreal, the CHU Sainte-Justine Research Centre in Montreal, Pepperdine University, Oklahoma State University, George Mason University, the University of Tennessee, the University of Chicago, the University of Vermont, and the Argonne National Laboratory, Macklin will be modeling infections in lung and gut tissues, allowing researchers to understand and test interventions. Using the models, researchers can study “what if” scenarios that can identify vulnerabilities in viral replication and the spread of infection while also seeking approaches that can control the immune response to avoid adverse reactions.
The research progressed quickly. How fast? Macklin first created his model late in the evening of March 25 after the rest of his family went to bed. The model included virus transport in the tissues, cell entry, replication, and release to infect nearby cells, and individual cell death in response to viral load: the key features of SARS-CoV-2 dynamics in a tissue prior to inflammation and immune involvement.
“By the morning, the basic model was working, and we had a web interactive version soon thereafter,” Macklin said. “We went from zero code and an empty notepad to a cloud-hosted model in 12 hours, showing that rapid prototyping was definitely feasible.”
Macklin live-tweeted his progress on the first night, and several researchers reached out in response, including a pharmacologist in private industry who offered to share immunology and angiotensin-converting enzyme 2—an enzyme that serves as the main entry point into cells for SARS-CoV-2—experience and data.
“Over the course of a couple of days, we were able to build in international coalition with a broad range of experience in virology, quantitative systems pharmacology, high performance computing, immunology, cloud computing, infectious disease modeling, tissue damage, inflammation, and simulation modeling,” Macklin said. “With this broad, multidisciplinary group’s diverse and complementary expertise, I knew we would be ready to make a difference.”
By working in collaboration with a wide range of experts in their respective fields, researchers can rapidly prototype models to arrive at potential answers quicker than if they were working on their own.
“The model we are building is a community resource: it is fully open source and available to all for their research projects,” Macklin said. “This allows the maximum benefit of the coalition’s collaboration, and it also encourages the community to share best results, parameter estimates, and data. This way, we can all work together and pool our expertise and experience to much more rapidly attack COVID-19. We also know that SARS-CoV-2 will not be the last novel pathogen or pandemic we will face. After we build this coalition and community resource, it will be available for the next health crisis. We won’t have to do this rapid crash prototyping project but can instead move straight to progress.”
The models will allow researchers to understand and test interventions in the coupled dynamics of COVID-19, including virus spread in tissue; virion adhesion to ACE2 receptors on cells; endocytosis (active transport into the cell); viral uncoating, replication, and assembly into new virions; viral exocytosis (release of completed virions); single-cell responses to infection, including disrupted metabolism, secretion of interferons, and cell death; inflammatory responses; immune activation and expansion in lymph nodes; immune cell infiltration and predation in infected tissue; and tissue damage, including edema that can lead to acute respiratory distress syndrome (ARDS).
“Using computer modeling to better understand how to combat COVID-19 allows us to respond with more agility to the challenge we’re facing,” said Kay Connelly, the associate dean for research at the Luddy School. “Paul’s previous research provided a great foundation for this type of work, and his ability to bring together other researchers from around North America to work on this critical problem is a perfect example of our mission of using technology to solve real-world issues.”

